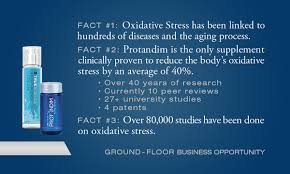
Protandim and Oxidavtive Stress
Oxidative Stress
Medical Research on Oxidative Stress and it’s direct link of effects to our bodies has exploded over the past five years. The National Institute of Health’s website www.pubmed.gov shows well over 120,000 medical research articles in peer reviewed publications. Simply go to www.pubmed.gov or scholar.google.com and type in oxidative stress in the search box.
To find out more about a particular condition and whether there is any research linking it with Oxidative Stress you can type in Oxidative Stress and the name of the condition. For instance you can find out about Oxidative Stress and Autism by typing in “Oxidative Stress Autism” in the search box. Further information can also be found at www.mylifevantage.com/thomasrbrown
What causes Oxidative Stress?
Have you ever cut an apple in half and seen how quickly it turns brown? Perhaps you’ve seen how quickly rust can form on a steel can that got wet and was left outside for a day? This is oxidation. Oxygen is life giving, and we could not live without it. However, oxygen also causes stress within your body.
Our body produces large numbers of dangerous and destructive “free radical” oxygen molecules just because we eat and breathe. Our blood stream is filled with these free-radicals all the time. Free radicals are unstable molecules that damage or “oxidize” cells throughout our body, and is called oxidative stress. The destructive power of these “free radicals” comes from the fact that each of these free radicals has a single un-paired electron. These unbalanced molecules need another electron to balance themselves out. As such, these unstable particles “steal” electrons from other parts of the body, which in turn damages genes, proteins and lipoproteins. Over time, this damage can render our cells and tissues unable to function properly. The damage that is caused, raises your risk of heart disease and cancer.
Antioxidants provide the electrons needed to stop the unbalanced molecules from stealing electrons from other parts of the body. Oxidative stress occurs when your body’s natural antioxidant defenses are overwhelmed because there are just too many free radicals in your system. We simply can’t stop this process, our bodies continually produce these free radicals naturally when we breathe, digest food and neutralize alcoholic and drugs of any type, and even when cells convert fat and carbohydrates into energy. When free radicals attack LDL cholesterol, it converts into the form that promotes atherosclerosis.
Free radicals are a byproduct of energy consumption in our mitochondria, the factories that produce energy in each of our cells. As we breathe, we can’t help but make some free radicals, but many other things factor into their production, your lifestyle and environment can also contribute. Some of the things that contribute to free radical formation are as follows:
Eating too many calories, sugars and/or refined carbohydrates. When we eat more, our mitochondria release more “exhaust,” creating higher levels of free radicals as they burn fuel from food for energy.
Exercising too much or too little. Exercise is an important part of any healthy lifestyle, but too much can increase oxidative stress in our bodies. In general, more than 60 minutes per day is considered excessive, while less than 30 minutes five times a week is not enough.
Excessive alcohol consumption. Drinking alcohol increases your levels of cytokines, inflammatory molecules that are linked to oxidative stress.
Exposure to tobacco smoke. Tobacco smoke contains more than 4,000 toxic chemicals that lead to oxidative stress.
Exposure to air pollutants. Allergens and industrial pollution increase oxidation in our bodies.
Excessive stress. Stress and the stress hormone cortisol increase inflammation, which further increases free radical production.
Ionizing radiation. Exposure to the sun, x-rays, radon, hair dryers, cellphones, airplanes, electric blankets and waterbed heaters can contribute to oxidative stress.
Eating charbroiled foods. These contain polycyclic aromatic hydrocarbons, which can contribute to oxidative stress.
Exposure to fungal toxins. Environmental molds (like those in bathrooms and basements) and internal molds and fungi (those related to your gut) can produce toxins that increase oxidative stress.
Poor liver and gut detoxification. When the liver becomes overwhelmed with toxins from food (like when you eat too much sugar) or the environment (like exposure to pesticides or mercury), it becomes inflamed and produces more free radicals.
Chronic infections. Dental infections and chlamydia can cause hidden infections that contribute to oxidative stress.
Lack of sleep. Sleep deprivation increases oxidation.
Oxidative stress and diseases:
Oxidative stress is an imbalance between the body generating free radicals and it’s ability to dispose of those free radicals (detoxify) prior to cellular damage.
The production of peroxides and free radicals damage all components of the cell, including proteins, lipids, and DNA. Thus, oxidative stress can cause disruptions in normal mechanisms of cellular signaling.
“In humans, oxidative stress is thought to be involved in the development of cancer,[1] Parkinson’s disease, Alzheimer’s disease,[2] atherosclerosis, heart failure,[3] myocardial infarction,[4][5] fragile X syndrome,[6] Sickle Cell Disease,[7] lichen planus,[8] vitiligo,[9] autism,[10] and chronic fatigue syndrome.[11]
Oxidative stress is suspected to be important in neurodegenerative diseases including Lou Gehrig’s disease (aka MND or ALS), Parkinson’s disease, Alzheimer’s disease, and Huntington’s disease.[27] Indirect evidence via monitoring biomarkers such as reactive oxygen species, and reactive nitrogen species production, antioxidant defense indicates oxidative damage may be involved in the pathogenesis of these diseases,[28][29] while cumulative oxidative stress with disrupted mitochondrial respiration and mitochondrial damage are related with Alzheimer’s disease, Parkinson’s disease, and other neurodegenerative diseases.[30]
Oxidative stress is thought to be linked to certain cardiovascular disease, since oxidation of LDL in the vascular endothelium is a precursor to plaque formation. Oxidative stress also plays a role in the ischemic cascade due to oxygen reperfusion injury following hypoxia. This cascade includes both strokes and heart attacks. Oxidative stress has also been implicated in chronic fatigue syndrome.[31] Oxidative stress also contributes to tissue injury following irradiation and hyperoxia, as well as in diabetes.
Oxidative stress is likely to be involved in age-related development of cancer. The reactive species produced in oxidative stress can cause direct damage to the DNA and are therefore mutagenic, and it may also suppress apoptosis and promote proliferation, invasiveness and metastasis.[1]Infection by Helicobacter pylori which increases the production of reactive oxygen and nitrogen species in human stomach is also thought to be important in the development of gastric cancer.[32]” Above quoted information and research was performed by the NutriFusion Company.
According to researchers oxidative stress may possibly be what switches atherosclerosis from ‘off’ to ‘on’. You will have read about LDL already on this website, and how it is considered the “bad” cholesterol. The critical thing to learn about oxidative stress is about when LDL particles become oxidized themselves. Low density lipoproteins carry a greater amount of fat (cholesterol) than their HDL brothers, but once they become oxidized, their cargo of cholesterol becomes more deadly. Oxidized LDL (LDL-ox ) can much more readily penetrate artery walls and end up forming artery-clogging plaque.
Your immune system’s cells called macrophages recognize these oxidized LDL’s as foreign invaders and trap them so that they become foam-filled cells that lay the foundation for plaque. LDL-ox end up making plaque grow larger and more rapidly, and eventually lead to major risk for clots, thrombosis and a stroke. Japanese research discovered that high levels of LDL-ox can more than double your risk of a heart attack! They also found out that those who did have a heart attack had levels of LDL-oxup to four times higher than those in the healthy heart group.
Doctors who understand oxidative stress today know that reducing a person’s risk of heart disease is much more than just “lowering cholesterol” – it is more about preventing oxidative stress by encouraging their patients to eat a diet rich in antioxidants, fruits and vegetables. These are the foods richest in antioxidants and therefore most likely to confer benefits, reducing the risk of oxidative stress.
So why not just take anti-oxidant supplements?
So why not just take antioxidant supplements – Vitamin C, E, CoQ10, etc? Or eat antioxidant rich foods such as blueberries or better yet the high anti-oxidant food, dark chocolate? When you research the effectiveness of anti-oxidants in fighting Oxidative Stress no single anti-oxidant can reduce Oxidative Stress enough to even measure. This is primarily because there are somewhere around 100 Trillion cells in each of our bodies and each day there are about 3×1023 free radicals generated in our cells. That is 300,000,000,000,000,000,000,000 free radicals. Since anti-oxidants work on a 1 to 1 ratio of anti-oxidants to free radicals we would have to eat something like 31 pounds of strawberries or 11 pounds of blueberries each and every day to be able to effectively reduce the free radicals using antioxidants only. When it comes to dark chocolate some may say they would like to eat as much as they can to fight the free radicals. Even if we could, our body would not be able to digest that much of those foods. Antioxidant supplements work on a one-to-one ratio. In other words for every antioxidant molecule ingested, you remove one free radical.
There is a way to fight and win!
What would you do if you could reduce the free radicals at a rate of one anti-oxidant to remove one million free radicals per second. Protandim works at this rate. For more information go to thomasrbrown.lifevantage.com
So there is a way to fight and win the battle each of us are in with Oxidative Stress.
Protandim (maybe the worlds best kept secret) is an all natural, herbal supplement that is clinically proven to reduce Oxidative Stress and increase our body’s own production of anti-oxidants., especially the super anti-oxidant Glutathione.
Learn more at thomasrbrown.lifevantage.com
References from NutriFusion Study
1. ^ a b Halliwell, Barry (2007). “Oxidative stress and cancer: have we moved forward?”. Biochem. J. 401 (1): 1–11. doi:10.1042/BJ20061131.PMID 17150040.
2. ^ Valko, M., Leibfritz, D., Moncol, J., Cronin, MTD., Mazur, M., Telser, J. (August 2007). “Free radicals and antioxidants in normal physiological functions and human disease”. International Journal of Biochemistry & Cell Biology 39 (1): 44–84. doi:10.1016/j.biocel.2006.07.001.PMID 16978905.
3. ^ Singh, N., Dhalla, A.K., Seneviratne, C., Singal, P.K. (June 1995). “Oxidative stress and heart failure”. Molecular and Cellular Biochemistry 147(1): 77–81. doi:10.1007/BF00944786.
4. ^ Ramond A, Godin-Ribuot D, Ribuot C, Totoson P, Koritchneva I, Cachot S, Levy P, Joyeux-Faure M. (December 2011). “Oxidative stress mediates cardiac infarction aggravation induced by intermittent hypoxia.”. Fundam Clin Pharmacol. doi:10.1111/j.1472-8206.2011.01015.x.PMID 22145601.
5. ^ Dean OM, van den Buuse M, Berk M, Copolov DL, Mavros C, Bush AI. (July 2011). “N-acetyl cysteine restores brain glutathione loss in combined 2-cyclohexene-1-one and D-amphetamine-treated rats: relevance to schizophrenia and bipolar disorder”. Neurosci Lett. 499 (3): 149–53.doi:10.1016/j.neulet.2011.05.027. PMID 21621586.
6. ^ de Diego-Otero Y, Romero-Zerbo Y, el Bekay R, Decara J, Sanchez L, Rodriguez-de Fonseca F, del Arco-Herrera I. (March 2009). “Alpha-tocopherol protects against oxidative stress in the fragile X knockout mouse: an experimental therapeutic approach for the Fmr1 deficiency.”.Neuropsychopharmacology 34 (4): 1011–26. doi:10.1038/npp.2008.152. PMID 18843266.
7. ^ Amer, J., Ghoti, H., Rachmilewitz, E., Koren, A., Levin, C. and Fibach, E. (January 2006). “Red blood cells, platelets and polymorphonuclear neutrophils of patients with sickle cell disease exhibit oxidative stress that can be ameliorated by antioxidants”. British Journal of Haematology 132(1): 108–113. doi:10.1111/j.1365-2141.2005.05834.x. PMID 16371026.
8. ^ Aly, D. G.; Shahin, R. S. (2010). “Oxidative stress in lichen planus”. Acta dermatovenerologica Alpina, Panonica, et Adriatica 19 (1): 3–11.PMID 20372767. edit
9. ^ Arican, O.; Kurutas, EB. (Mar 2008). “Oxidative stress in the blood of patients with active localized vitiligo.”. Acta Dermatovenerol Alp Panonica Adriat 17 (1): 12–6. PMID 18454264.
10. ^ James, SJ.; Cutler, P.; Melnyk, S.; Jernigan, S.; Janak, L.; Gaylor, DW.; Neubrander, JA. (Dec 2004). “Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism.”. Am J Clin Nutr 80 (6): 1611–7. PMID 15585776.
11. ^ Gwen Kennedy, Vance A. Spence, Margaret McLaren, Alexander Hill, Christine Underwood & Jill J. F. Belch (September 2005). “Oxidative stress levels are raised in chronic fatigue syndrome and are associated with clinical symptoms”. Free radical biology & medicine 39 (5): 584–9.doi:10.1016/j.freeradbiomed.2005.04.020. PMID 16085177.
12. ^ Segal, AW (2005). “How neutrophils kill microbes”. Annu Rev Immunol 9 (5): 197–223. doi:10.1146/annurev.immunol.23.021704.115653.PMC 2092448. PMID 15771570.
13. ^ Gems D, Partridge L (March 2008). “Stress-response hormesis and aging: “that which does not kill us makes us stronger””. Cell Metab. 7(3): 200–3. doi:10.1016/j.cmet.2008.01.001. PMID 18316025.
14. ^ Schafer FQ, Buettner GR (2001). “Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple”. Free Radic. Biol. Med. 30 (11): 1191–212. doi:10.1016/S0891-5849(01)00480-4. PMID 11368918.
15. ^ Lennon SV, Martin SJ, Cotter TG (1991). “Dose-dependent induction of apoptosis in human tumour cell lines by widely diverging stimuli”. Cell Prolif. 24 (2): 203–14. doi:10.1111/j.1365-2184.1991.tb01150.x. PMID 2009322.
16. ^ Valko M, Morris H, Cronin MT (May 2005). “Metals, toxicity and oxidative stress”. Curr. Med. Chem. 12 (10): 1161–208.doi:10.2174/0929867053764635. PMID 15892631.
17. ^ Evans MD, Cooke MS (May 2004). “Factors contributing to the outcome of oxidative damage to nucleic acids”. BioEssays 26 (5): 533–42.doi:10.1002/bies.20027. PMID 15112233.
18. ^ LC Colis, P Raychaudhury, AK Basu (2008). “Mutational specificity of gamma-radiation-induced guanine-thymine and thymine-guanine intrastrand cross-links in mammalian cells and translesion synthesis past the guanine-thymine lesion by human DNA polymerase eta”.Biochemistry 47 (6): 8070–9. doi:10.1021/bi800529f. PMID 18616294.
19. ^ Lelli JL, Becks LL, Dabrowska MI, Hinshaw DB (1998). “ATP converts necrosis to apoptosis in oxidant-injured endothelial cells”. Free Radic. Biol. Med. 25 (6): 694–702. doi:10.1016/S0891-5849(98)00107-5. PMID 9801070.
20. ^ Lee YJ, Shacter E (1999). “Oxidative stress inhibits apoptosis in human lymphoma cells”. J. Biol. Chem. 274 (28): 19792–8.doi:10.1074/jbc.274.28.19792. PMID 10391922.
21. ^ Sies, H. (1985). “Oxidative stress: introductory remarks”. In H. Sies, (Ed.). Oxidative Stress. London: Academic Press. pp. 1-7.
22. ^ Docampo, R. (1995). “Antioxidant mechanisms”. In J. Marr and M. Müller, (Eds.). Biochemistry and Molecular Biology of Parasites. London: Academic Press. pp. 147-160.
23. ^ a b Rice-Evans CA, Gopinathan V (1995). “Oxygen toxicity, free radicals and antioxidants in human disease: biochemical implications in atherosclerosis and the problems of premature neonates”. Essays Biochem. 29: 39–63. PMID 9189713.
24. ^ Seaver LC, Imlay JA (November 2004). “Are respiratory enzymes the primary sources of intracellular hydrogen peroxide?”. J. Biol. Chem. 279(47): 48742–50. doi:10.1074/jbc.M408754200. PMID 15361522.
25. ^ Messner KR, Imlay JA (November 2002). “Mechanism of superoxide and hydrogen peroxide formation by fumarate reductase, succinate dehydrogenase, and aspartate oxidase”. J. Biol. Chem. 277 (45): 42563–71. doi:10.1074/jbc.M204958200. PMID 12200425.
26. ^ Imlay JA (2003). “Pathways of oxidative damage”. Annu. Rev. Microbiol. 57: 395–418. doi:10.1146/annurev.micro.57.030502.090938.PMID 14527285.
27. ^ Patel VP, Chu CT. (2011). “Nuclear transport, oxidative stress, and neurodegeneration.”. Int J Clin Exp Pathol. 4 (3): 215–29. PMC 3071655.PMID 21487518.
28. ^ Nunomura A, Castellani RJ, Zhu X, Moreira PI, Perry G, Smith MA. (2005). “Involvement of oxidative stress in Alzheimer disease.”. J Neuropathol Exp Neurol. 65 (7): 631–41. doi:10.1097/01.jnen.0000228136.58062.bf. PMID 16825950.
29. ^ Bošković M, Vovk T, Kores Plesničar B, Grabnar I. (2011). “Oxidative stress in schizophrenia”. Curr Neuropharmacol. 9 (2): 301–12.doi:10.2174/157015911795596595. PMC 3131721. PMID 22131939.
30. ^ Ramalingam M, Kim SJ. (2012). “Reactive oxygen/nitrogen species and their functional correlations in neurodegenerative diseases”. Journal of Neural Transmission 119. doi:10.1007/s00702-011-0758-7. PMID 22212484.
31. ^ Nijs J, Meeus M, De Meirleir K (2006). “Chronic musculoskeletal pain in chronic fatigue syndrome: recent developments and therapeutic implications.”. Man Ther 11 (3): 187–91. doi:10.1016/j.math.2006.03.008. PMID 16781183.
32. ^ Handa O, Naito Y, Yoshikawa T. (2011). “Redox biology and gastric carcinogenesis: the role of Helicobacter pylori”. Redox Rep. 16 (1): 1–7.doi:10.1179/174329211X12968219310756. PMID 21605492.
33. ^ Meyers DG, Maloley PA, Weeks D (1996). “Safety of antioxidant vitamins”. Arch. Intern. Med. 156 (9): 925–35. doi:10.1001/archinte.156.9.925.PMID 8624173.
34. ^ Ruano-Ravina A, Figueiras A, Freire-Garabal M, Barros-Dios JM (2006). “Antioxidant vitamins and risk of lung cancer”. Curr. Pharm. Des. 12 (5): 599–613. doi:10.2174/138161206775474396. PMID 16472151.
35. ^ Pryor WA (2000). “Vitamin E and heart disease: basic science to clinical intervention trials”. Free Radic. Biol. Med. 28 (1): 141–64.doi:10.1016/S0891-5849(99)00224-5. PMID 10656300.
36. ^ Boothby LA, Doering PL (2005). “Vitamin C and vitamin E for Alzheimer’s disease”. Ann Pharmacother 39 (12): 2073–80.doi:10.1345/aph.1E495. PMID 16227450.
37. ^ Kontush K, Schekatolina S (2004). “Vitamin E in neurodegenerative disorders: Alzheimer’s disease”. Ann. N. Y. Acad. Sci. 1031: 249–62.doi:10.1196/annals.1331.025. PMID 15753151.
38. ^ Fong JJ, Rhoney DH (2006). “NXY-059: review of neuroprotective potential for acute stroke”. Ann Pharmacother 40 (3): 461–71.doi:10.1345/aph.1E636. PMID 16507608.
39. ^ Larsen PL (1993). “Aging and resistance to oxidative damage in Caenorhabditis elegans”. Proc. Natl. Acad. Sci. U.S.A. 90 (19): 8905–9.doi:10.1073/pnas.90.19.8905. PMC 47469. PMID 8415630.
40. ^ Helfand SL, Rogina B (2003). “Genetics of aging in the fruit fly, Drosophila melanogaster”. Annu. Rev. Genet. 37: 329–48.doi:10.1146/annurev.genet.37.040103.095211. PMID 14616064.
41. ^ Publication demonstrating that oxidative stress is promoting life span
42. ^ Tapia PC (2006). “Sublethal mitochondrial stress with an attendant stoichiometric augmentation of reactive oxygen species may precipitate many of the beneficial alterations in cellular physiology produced by caloric restriction, intermittent fasting, exercise and dietary phytonutrients: “Mitohormesis” for health and vitality”. Med. Hypotheses 66 (4): 832–43. doi:10.1016/j.mehy.2005.09.009. PMID 16242247.
43. ^ Sohal RS, Mockett RJ, Orr WC (2002). “Mechanisms of aging: an appraisal of the oxidative stress hypothesis”. Free Radic. Biol. Med. 33 (5): 575–86. doi:10.1016/S0891-5849(02)00886-9. PMID 12208343.
44. ^ Sohal RS (2002). “Role of oxidative stress and protein oxidation in the aging process”. Free Radic. Biol. Med. 33 (1): 37–44. doi:10.1016/S0891-5849(02)00856-0. PMID 12086680.
45. ^ Rattan SI (2006). “Theories of biological aging: genes, proteins, and free radicals”. Free Radic. Res. 40 (12): 1230–8.doi:10.1080/10715760600911303. PMID 17090411.
46. ^ Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C (2007). “Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: systematic review and meta-analysis”. JAMA 297 (8): 842–57. doi:10.1001/jama.297.8.842. PMID 17327526.. See also the letter to JAMA by Philip Taylor and Sanford Dawsey and the reply by the authors of the original paper.
48. ^ Devasagayam, TPA; Tilac JC, Boloor KK, Sane Ketaki S, Ghaskadbi Saroj S, Lele RD (October 2004). “Free Radicals and Antioxidants in Human Health: Current Status and Future Prospects”. Journal of Association of Physicians of India 52: 796.
47. ^ *Pratviel, Genevieve (2012). “Chapter 7. Oxidative DNA Damage Mediated by Transition Metal Ions and Their Complexes”. In Astrid Sigel, Helmut Sigel and Roland K. O. Sigel. Interplay between Metal Ions and Nucleic Acids. Metal Ions in Life Sciences 10. Springer. pp. 201–216.doi:10.1007/978-94-007-2172-2_7.
49. ^ Nathan C, Shiloh MU (2000). “Reactive oxygen and nitrogen intermediates in the relationship between mammalian hosts and microbial pathogens”. Proc. Natl. Acad. Sci. U.S.A. 97 (16): 8841–8. doi:10.1073/pnas.97.16.8841. PMC 34021. PMID 10922044.